Introduction: Multiple myeloma (MM) is an incurable hematologic malignancy caused by the neoplastic proliferation of plasma cells within the bone marrow. The tumor microenvironment within the bone marrow consists of a diverse array of immune cells which regulate MM cell proliferation and survival. Specifically, tumor-associated macrophages (TAMs) derived from peripheral blood monocytes migrate to the bone marrow where they support MM cell growth and promote resistance to apoptosis. Several studies suggest that the amount of bone marrow TAMs directly correlates with disease activity and worse clinical outcomes in MM. Considering that peripheral blood absolute monocyte count (AMC) could reflect the burden of bone marrow TAMs, we sought to determine the prognostic significance of AMCs at diagnosis of MM.
Methods: Using the integrated nationwide VA electronic health records and VA Corporate Data Warehouse, patients were identified by International Classification of Diseases (ICD) codes for MM. Patients were required to have at least 3 visits with an MM ICD code on separate days, have received at least one MM drug with the exception of corticosteroids after the date of diagnosis and have 2 or more absolute monocyte counts measured by automated or manual differential at separate visits within 18 months before and 7 days after MM diagnosis. We further confirmed the date of diagnosis using the VA Cancer Registry. We excluded patients with aplastic anemia, myelodysplastic syndrome, chronic myelomonocytic leukemia and other myeloproliferative neoplasms. In this cohort, monocytosis was defined based on the institution's cut-off as a sustained absolute increase in monocyte count of 0.8 (800/mm3) or greater with extreme monocytosis being greater than 1.25 (1250/mm3). Patients were stratified into three groups according to AMC at diagnosis, namely AMC <0.8, AMC 0.8 - 1.25 and AMC >1.25. To avoid extreme values significantly affecting the analysis, the Kruskal-Wallis test was used to compare continuous variables between the groups. Chi-squared tests were used to compare categorical variables. Hazard estimates for the prognostic analysis were obtained via adjusted Cox proportional hazard models. Overall survival was estimated using the Kaplan-Meier method and log-rank tests were used to compare the survival of each group.
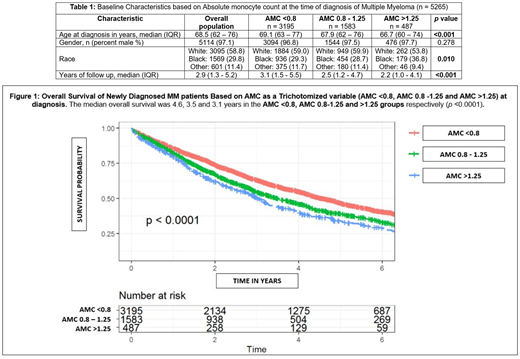
Results: A total of 5,265 patients with MM were included in the final analysis with a median follow up of 2.9 years (range 1.3 - 5.2). At diagnosis of MM, 39.3% of patients presented with monocytosis. Patients with monocytosis were younger and more likely to have abnormal levels of prognostic markers known to be associated with increased tumor burden and worse outcomes in MM. Notably, patients with monocytosis had higher median levels of β2-microglobulin and lactate dehydrogenase (p <0.001) and lower median albumin levels (p <0.001) than those without monocytosis. Patients with extreme monocytosis had the highest median β2-microglobulin (5.01, range 3.30 - 6.98, p <0.001) and the lowest median albumin levels (2.9, range 2.4 - 3.4, p <0.001) in the entire cohort. Patient characteristics according to AMC at diagnosis are shown in Table 1. On univariate analysis, the AMC predicted overall survival when analyzed as a trichotomized variable. The median overall survival was 4.6, 3.5 and 3.1 years in the AMC <0.8, AMC 0.8-1.25 and AMC >1.25 groups respectively (p <0.0001) [Figure 1]. When adjusting for known prognostic factors associated with outcomes in MM, the AMC was significantly associated with inferior overall survival (AMC 0.8 - 1.25 HR 1.230, p <0.008; AMC >1.25 HR of 1.312, p <0.003).
Conclusion: The results of our study suggest that an elevated absolute monocyte count at MM diagnosis is associated with worse overall survival independent of known poor prognostic factors. The role of peripheral blood monocyte count as a surrogate biomarker for the state of the bone marrow microenvironment in MM warrants further in vitro, prospective studies.
Munshi:AbbVie: Consultancy; Amgen: Consultancy; Legend: Consultancy; Adaptive: Consultancy; Janssen: Consultancy; C4: Current equity holder in private company; OncoPep: Consultancy, Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Karyopharm: Consultancy; Takeda: Consultancy; BMS: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal